What can the (specialized) physical therapist mean for this pain suffering group.

Introduction
According to “The Global Burdon of Diseases Study” (GBDS; Vos et al 2019) HA’s are one of the two most common causes of disability in the 10-24 year age group.
Singhi and colleagues mention that HA prevalence rises from 3-8% of 3-year-olds to 57-82% of 8-15-year-old children (Singhi et al 2014).
Until the age of 11 there seems to be no gender differences, while in children older than 11 years HA seem to be more common in girls. Socioeconomic status has no relationship with pediatric HA; however, there is small evidence that HA is more common in single-parent households. Children with HA who present with other pain complaints, have more chronic diseases and psychologic problems. For example, children with migraine suffer more often from abdominal pain and back pain (Kröner-Herwig et al 2007). Therefore, children with migraine use more medical care than children with TTH (Arruda et al 2010).
The question arises, is there an increase in the prevalence of HA in children in the last decades? This question cannot be answered clearly. According to the GBDS HA in the age group 10-24 years was increasing from third most common disease in 1990 to second most common disease in 2019 (Vos et al 2019). In an overview article from Albers et al in 2015 they found evidence in 4 studies of some (varying) increase in the prevalence of HA in the last decades, with higher rates for girls but no geographic differences.
The diagnosis of HA can only be made by evaluation of the child’s signs and symptoms with the use of “The International Classification of Headache Disorders, 3rd edition” (ICHD-3; Arnold 2018) which describes different HA types in adults and children.
The International Classification of Headache Disorders, 3rd edition” (ICHD-3- 2018)
The classification distinguishes between Primary HA, Secondary HA and the group of painful cranial neuropathies, other facial pain and other HA’s (see Figure 1).
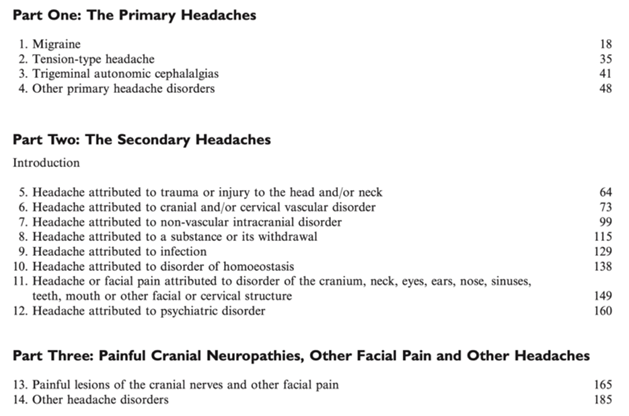
Figure 1, Content of The International Classification of Headache Disorders, 3rd edition, page 4 (Arnold 2018).
The classification describes primary the different HA types in adults. When here is substantial evidence, different and/ or additional facts for HA in children, it is described.

What is different in children?
Here are some of the special features for children with HA mentioned in the ICHD-3 and literature.
Primary HA
In migraine without aura in children the duration of the attack may last 2-72 hours, the pain localization is more often bilateral and usually located frontotemporal. Occipital headache in children is rare and calls for diagnostic caution.
In migraine with aura there is no difference mentioned between adults and children, while in literature this type of HA seems to be rare in children and if present, visual disturbances are most often described (Kröner-Herwig et al 2007).
Special HA- types in children
The chapter 1.6 “Episodic syndromes that may be associated with migraine” highlights 4 different types of HA which occur mostly in children (see also figure 2):
Recurrent gastrointestinal disturbance (1.6.1)
- Cyclic vomiting syndrome (1.6.1.1) In this syndrome children have intense nausea and vomiting attacks of a certain amount without gastrointestinal dysfunctions or diseases.
- Abdominal migraine (1.6.1.2) In this syndrome children have a certain amount of attacks of abdominal pain and associated symptoms or signs (anorexia, nausea, vomiting, pallor) without gastrointestinal or renal diseases.
In both syndromes’ children are young at onset (before 6 years, Prakash et al 2001) and have a high chance to develop migraine later in life (Arnold 2018, Li and Balint 2000).
Benign paroxysmal vertigo (1.6.2) Young Children (onset between 2-4 years, Lindskog et al 1999) have sudden vertigo attacks with associated symptoms (nystagmus, ataxia, vomiting, pallor, fearfulness) which resolve spontaneously after minutes or hours without loss of consciousness (Arnold 2018).
Benign paroxysmal torticollis (1.6.3) This syndrome appears in young children (2-6 months, Rosman et al 2009) with attacks of the head tilt to one side and accompanied of associated symptoms (pallor, irritability, malaise, vomiting, ataxia) without neurological findings.
Additional pediatric HA- types
In the appendix of the ICHD-3 there are additional three pediatric HA types mentioned, with some evidence, but not enough to be listed in the main part of the classification:
- Infantile colic (A 1.6.4) Characterized with recurrent episodes of irritability, fussing or crying from birth to four months of age for a certain amount of time of an otherwise healthy and well- fed infant.
- Alternating hemiplegia of childhood (A 1.6.5) Alternating hemiplegia starting before 18 month of age and at least one other sign of paroxysmal phenomenon and evidence of mental and/or neurological deficit(s).
- Vestibular migraine (A 1.6.6) Vestibular symptoms together with migrainous features which can occur at any age.

Figure 2, Age-related expression of childhood episodic syndromes common precursors of migraine. *Infantile colic is actually considered as an episodic syndrome than may be associated with migraine (from Spiri et al 2014).
There are no further differences between adults and children mentioned for Tension-type HA, Trigeminal autonomic cephalalgias and other primary HA disorders; however, the last two are very uncommon in children (Lewis 2007).
Secondary HA
The exact prevalence of secondary HA in children is not known.
The most frequently identified etiology of secondary headache in children is viral infections (29-30%), in particular respiratory tract infections, or minor head trauma; in a small minority of patient’s headaches are secondary to serious life-threatening intracranial disorders (Celle et al 2010). While uncommon in children, subarachnoid hemorrhages do occur, particularly in those with risk factors such as a coagulopathy, sickle cell disease, or hypertension (Lewis 2007).
Critical note on de ICHD-3 classification
According to this classification tension-type headache (TTH) occurs more often than migraine (respectively 18,5% and 7,5%), but unclassifiable HA is most common (27%; Kröner-Herwig et al 2007). This finding points out some weakness of the international classification in the judgement of pediatric HA. There are critical notes about the described duration of pain attacks with a minimum of 2 hours which should be decreased to a minimum of 30 minutes (McAbee et al 2016). The described pulsating character of adult migraine is infrequent in younger children but increasingly reported with increasing age (Rossi et al 2008) and then pulsating is often accompanied with pressing (Trottier et al 2013). There is also a proposal for mention of family history of HA, because there seem to be a higher prevalence of HA in children if one parent also has a history of HA (72,3% in comparison with no parental HA with 27,7%; Kröner-Herwig et al 2007).
Pathophysiology of (recurrent or persistent) pediatric HA
The pathophysiology behind HA is mainly described for adults and there are different models of explanation. Several studies have identified the role of some genes in the pathophysiology of migraine (Gormley et al 2016); however, epigenetic mechanisms may play an important role in the etiology and phenotypic expression of migraine disorders, and these mechanisms may explain how non-genetic factors (such as female hormones, stress, and inflammation) may modulate the severity and frequency of the attacks (Figure 3, Eising et al 2013).
Slover and Kent (2015) describe 2 current explanations- the vasogenic theory which referees to the involvement of extracranial and intracranial vessels- and the neurovascular theory which shows an altered cerebral susceptibility.
However, research shows involvement of the cerebral cortex and the trigemino-vascular system (Burstein et al 2005). The migrainous brain is characterized by a lack of habituation (cortical dysfunction and abnormal thalamic activity) of evoked responses to repeated stimuli (Coppola et al 2009) which can be due to changes in the number of neuropeptides/neurotransmitters (Noseda et al 2014).
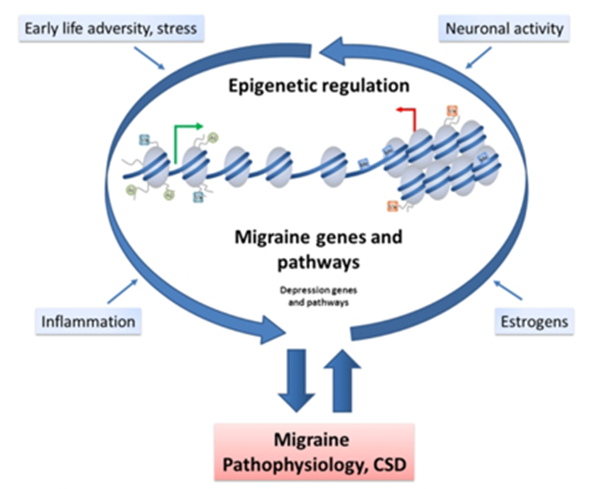
Figure 3, Proposed model in which epigenetic factors influence migraine pathophysiology (from Eising et al 2013). CSD= cortical spreading depression.
Additional factors in HA in children
Not every child has the same probability of getting (chronic) HA. There seem to exist some other facts and/or health issues which can play a certain part in children and the probability of getting HA.
Some of these factors are called risk factors:
- Risk factors Literature points out that there are certain risk factors to develop pediatric (neck- and) HA: socio-emotional stress, female, sleeping difficulties and fatigue, HA as family disorder and decreased mobility of the upper and/or lower cervical spine (Driehuis et al 2017).
Health issues can also be called comorbidities:
- Comorbidities It is widely recognized that headache patients with comorbidity made a greater use of health services, and they have a poor health perception than headache patients without comorbidity. So, it is very important to recognize the presence of these comorbidities, because if they are not acknowledged, they could have a negative impact on adherence to treatment and quality of life, and they could increase the risk of headache chronicity (Minen et al 2016).
Proven comorbidities are: - Abuse
- ADHA and learning disorders
- Atopic disorders
- Brain tumors and epilepsy
- Psycho-emotional disorders
- Sleep disorders
- Autism spectrum disorders
- Obesity
- Musculoskeletal dysfunctions
- Vestibular dysfunctions
Special attention for (specialized) physical therapists:
Evidence points out that there are some points of attention (specialized) physical therapist can focus on while assessing and treating children with HA:
- Obesity: The majority of data points to a positive association between headache (especially migraine) and obesity among children and adolescents (Guidetti et al 2017).
- Musculoskeletal dysfunctions:
- TMD (Temporo-mandibular dysfunction):
- Adolescents (n= 149, 13-15 years) with painful TMD were more likely to have migraine compared with those without TMD (controls; odds ratio = 3.0) (Fernandes et al 2019).
- Adolescents (n=1307, 12-14 years) presenting with HAs were more likely to present painful TMD (OR = 4.94; P
- Children with bruxing or clenching habits and those with posterior crossbite have a greater likelihood of developing signs and symptoms of TMD (Pereira et al 2009).
- Posterior crossbite and overbite >5 mm was associated with significantly increased risk of headache (>3:1) in children and adolescents. The combination of 2 or 3 occlusal factors (overjet) increased the risk of headache even more (8.5:1) (Lambourne et al 2007).
- Cervical spine dysfunctions:
- Neck pain is associated with migraine but not with tension-type headache; n=1441, 12-19 years, (Blaschek et al 2014).
- Children with CTTH (Chronic Tensiontype headache) (n= 50, 5-11 years) showed decreased CROM as compared to children without headache (n=50) for flexion, extension, right- and left lateral- flexions, and total range of motion for flexion-extension and lateral-flexion but not for rotation or total range of motion for rotation (Fernandez-Mayoralas et al 2010).
- When compared to asymptomatic controls (n=34), symptomatic children (n=30, 6-12 years) had a significantly smaller CVA (Craniovertebral angle) less active ROM in all cardinal planes and less ROM during the FRT (Flexion-Rotation-Test), especially towards the dominant headache side. In addition, symptomatic subjects reported significantly more pain during the FRT and there was a significant negative correlation between the range recorded during the FRT towards the dominant headache side and FRT pain intensity score (Budelmann et al 2013).
- Traumatic injuries
- The prevalence of headache 3 months after injury was significantly higher after mTBI (mild traumatic brain injury) (n=402) than after AI (arm injury) (n=122, 5-17 years) in adolescents (13-17 years, 46% vs 25%) and in girls (5-12 years, 59% vs 24%). The prevalence of headache at 3 months was also higher after moderate/severe TBI (n=60) than AI in younger children (5–12 years, 60% vas 27%)). Twelve months after injury, TBI was not associated with a significantly increased frequency of headache. However, girls with mTBI reported serious headache (> 5 of 10 pain scale rating) more often than controls (Blume et al 2012).
- Vestibular dysfunctions:
- The most frequent diagnosis in children with vestibular complaints (n=147, 1-18 years) was MRV (migraine related vertigo, 28%), followed by MSV (migraine related and somatoform vertigo (SV), 19%) and SV alone (14%). MSV occurred most frequently in adolescent girls (25%) (Langhagen et al 2013).
What can a certificate CRAFTA® therapist do with children with headache?
The certificated CRAFTA® therapist is able to detect the kind of headache along with additional risk factors or comorbidities a child is presenting with. Every step of the evaluation and treatment will be practiced according to Clinical Reasoning principals (Jones 1992, 2018).
Therefore, a to-the-point and clear subjective evaluation will take place with the child and if necessary the family.
In the subjective evaluation there will be questions about possible red flags (Lewis 2007, Driehuis et al 2018, van der Meer et al 2018) so the therapist is able to plan (if necessary a referral and) a management pathway (Rajapakse et al 2014).
If there are no red flags the therapist will start the physical examination, which is divided into inspection and observation, palpation and clinical testing. If there are red flags or not clear conditions, the child has to be referred to the physician or specialist.
a. Inspection and observation of spine, head and face, muscle tone, skin, facial expression, body- extremities- and head movements and head-neck and body posture (Budelmann et al 2013, Mönch-Tegeter et al 2013);
b. Palpation for the identification of anatomical abnormalities, tissue changes;
c. Clinical testing of:
- general condition (length, weight and head circumference (infants, WHO 2007) motor function according to age (Henderson et al 2007, Brown 2019), (Figure 4)
- TMJ (active and passive movement (Hirsch et al 2006)), palpation and muscle function (Chaves et al 2010) and noise registration (Dagar et al 2006) (see also statement TMJ). (Figure 4)

Figure 4 a. Clinical testing of the active mouth opening with a ruler; b. clinical testing of the upper cervical spine with the FRT (Flexion-Rotation-Test) (pictures von Piekartz).
- cervical and upper cervical region (active (Arbogast et al 2007, Budelmann et al 2016) and passive movement (Budelmann et al 2013))
- vestibular system (Mönch-Tegeder et al 2013)
- (pheripheral) nervous system (general (Driehuis et al 2018), cranial nerves (von Piekartz et al 2015), neurodynamic testing (von Piekartz et al 2007))
- Cranial Compliance (see also “Statement craniofacial manual therapy” (von Piekartz et al 2015) Manual cranial therapy
Using the findings of the subjective evaluation, additional questions (van der Meer et al 2018), questionnaires (Driehuis et al 2018) and the physical examination a treatment plan will be formulated and discussed with the child (and thfamily).
Additional to the pharmacological treatment, which can be prescribed as acute (Slover and Kent 2015) and/or prophylactic treatment (Locher et al 2020), the (CRAFTA®) physical therapy treatment may include following treatment options:
- Behavioral therapy, for example:
- treatment adherence (Guidetti et al 2017, Bensing and Verheul 2010)
- lifestyle management (Slover and Kent 2015, Frag et al 2013)
- relaxation techniques and biofeedback (Slover and Kant 2015), biofeedback and virtual reality (Shiri et al 2013))
- Training (Baillie et al 2014)
- Pain education (Pincus et al 2013, Hurley-Wallace et al 2019)
- Treatment of musculoskeletal dysfunctions:
- Motor- and movement skills (exercise)
- TMD
- Cervical region (Figure 5)
- Craniofacial region
- (peripheral) nervous system (Neuraxis and /or cranial nerves)
- Vestibular system
- Oculomotor system

Figure 5 treatment technique for the upper cervical spine (picture von Piekartz).
Promising treatment in the future (until now evidence in adults, but not in children):
- Mirror therapy
- Laterality- and emotion (recognition) training (von Piekartz and Mohr 2014)
The CRAFTA® therapist, child and parents use a collaborative reasoning process to evaluate the changes in signs and symptoms according to the clinical parameters of the AAN (American Academy of Neurology Practice Parameter, Silberstein 2000)
These parameters are
- Reduction of headache frequency, severity, duration, and disability
- Reduction of reliance on poorly tolerated, ineffective, or unwanted acute pharmacotherapies
- Improvement in the quality of life
- Avoidance of acute headache medication escalation
- Education and enablement of patients to manage their disease to enhance personal control of their migraine; and
- Reduction of headache-related distress and psychological symptoms
If the signs and symptoms will not change and decrease for 20-30% during the first 3-4 treatments, the child has to be referred to a physician or specialist.
The specialized CRAFTA® therapist aims to work as part of an interdisciplinary team with medical doctors (pediatrician, neurologist, general doctor), speech therapists, psychological therapist and other disciplines to increase the outcome of the above mentioned parameters (Shulman et al 2020).
We will present more information of headache in adults of other dysfunctions in children at a later moment.
October 2022, Daniela von Piekartz, Harry von Piekartz
References
- Albers, L., von Kries, R., Heinen, F., & Straube, A. (2015). Headache in school children: is the prevalence increasing?. Current pain and headache reports, 19(3), 4.
- Arbogast, K. B., Gholve, P. A., Friedman, J. E., Maltese, M. R., Tomasello, M. F., & Dormans, J. P. (2007). Normal cervical spine range of motion in children 3–12 years old. Spine, 32(10), E309-E315.
- Arnold, M. (2018). Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia, 38(1), 1-211.
- Arruda, M. A., Guidetti, V., Galli, F., Albuquerque, R. C., & Bigal, M. E. (2010). Primary headaches in childhood–a population-based study. Cephalalgia, 30(9), 1056-1064.
- Baillie, L. E., Gabriele, J. M., & Penzien, D. B. (2014). A systematic review of behavioral headache interventions with an aerobic exercise component. Headache: The Journal of Head and Face Pain, 54(1), 40-53.
- Bensing, J. M., & Verheul, W. (2010). The silent healer: the role of communication in placebo effects. Patient education and counseling, 80(3), 293-299.
- Blaschek, A., Decke, S., Albers, L., Schroeder, A. S., Lehmann, S., Straube, A., ... & von Kries, R. (2014). Self-reported neck pain is associated with migraine but not with tension-type headache in adolescents. Cephalalgia, 34(11), 895-903.
- Blume, H. K., Vavilala, M. S., Jaffe, K. M., Koepsell, T. D., Wang, J., Temkin, N., ... & Rivara, F. P. (2012). Headache after pediatric traumatic brain injury: a cohort study. Pediatrics, 129(1), e31-e39.
- Brown, T. (2019). Structural validity of the Bruininks-Oseretsky test of motor proficiency–Second edition brief form (BOT-2-BF). Research in Developmental Disabilities, 85, 92-103.
- Budelmann, K., von Piekartz, H., & Hall, T. (2013). Is there a difference in head posture and cervical spine movement in children with and without pediatric headache?. European journal of pediatrics, 172(10), 1349-1356.
- Budelmann, K., Piekartz, H. V., & Hall, T. (2016). A normative study of cervical range of motion measures including the flexion–rotation test in asymptomatic children: side-to-side variability and pain provocation. Journal of Manual & Manipulative Therapy, 24(4), 185-191.
- Burstein, R., & Jakubowski, M. (2005). Unitary hypothesis for multiple triggers of the pain and strain of migraine. Journal of comparative neurology, 493(1), 9-14.
- Celle, M. E., Carelli, V., & Fornarino, S. (2010). Secondary headache in children. Neurological Sciences, 31(1), 81-82.
- Chaves, T. C., Nagamine, H. M., de Sousa, L. M., de Oliveira, A. S., & Grossi, D. B. (2010). Comparison between the reliability levels of manual palpation and pressure pain threshold in children who reported orofacial pain. Manual therapy, 15(5), 508-512.
- Coppola, G., Pierelli, F., & Schoenen, J. (2009). Habituation and migraine. Neurobiology of learning and memory, 92(2), 249-259.
- Dagar, S. R., Pakhan, A. J., Thombare, R. U., & Bhovar, A. (2006). Modified stethoscope for auscultation of temporomandibular joint sounds. The Journal of Indian Prosthodontic Society, 6(1), 29.
- Driehuis, F., Nijhuis-van de Sanden, M.W.G., Hoogeboom, T., Maisson, F., Overvelde A., van der Wees, G., Meurs, M. (2017). Rapport samenwerking tussen de manueel therapeut en kinderfysiotherapeut: uitkomsten van een enquête. https://nvfk.kngf2.nl/actueel/nieuws/2018/01-2018/rapport-samenwerking-tussen-de-manueel-therapeut-en-kinderfysiotherapeut-uitkomsten-van-een-enquete.html
- Driehuis, F., Nijhuis-van de Sande, M.W.G., Saedt, E.R.I.C., van der Woude, B.H., de Bie, R.A. (2018). Factsheet Manuele therapie en diagnostische mogelijkheden bij kinderen (1-18 jaar). And
Verantwoording Factsheet Manuele therapie en diagnostische mogelijkheden bij kinderen (1-18 jaar) https://nvmt.kngf2.nl/binaries/content/assets/bi/nvmt/onbeveiligd/vakgebied/factsheets/2018-04_nvmt_factsheet_mt-bij-kinderen-diagnose.pdf - Eising, E., Datson, N. A., van den Maagdenberg, A. M., & Ferrari, M. D. (2013). Epigenetic mechanisms in migraine: a promising avenue?. BMC medicine, 11(1), 26.
- Fernandes, G., Arruda, M. A., Bigal, M. E., Camparis, C. M., & Gonçalves, D. A. (2019). Painful temporomandibular disorder is associated with migraine in adolescents: a case-control study. The Journal of Pain, 20(10), 1155-1163.
- Fernández-Mayoralas, D. M., Fernández-de-las-Penas, C., Palacios-Cena, D., Cantarero-Villanueva, I., Fernández-Lao, C., & Pareja, J. A. (2010). Restricted neck mobility in children with chronic tension type headache: a blinded, controlled study. The Journal of headache and pain, 11(5), 399-404.
- Franco, A. L., Fernandes, G., Goncalves, D. A., Bonafé, F. S., & Camparis, C. M. (2014). Headache associated with temporomandibular disorders among young Brazilian adolescents. The Clinical journal of pain, 30(4), 340-345.
- Gormley, P., Anttila, V., Winsvold, B. S., Palta, P., Esko, T., Pers, T. H., ... & Kurth, T. (2016). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nature genetics, 48(8), 856-866.
- Guidetti, V., Arruda, M. A., & Ozge, A. (Eds.). (2017). Headache and comorbidities in childhood and adolescence. Springer International Publishing.
- Henderson, S. E., Sugden, D. A., & Barnett, A. L. (2007). Movement assessment battery for children-2 (2nd edn) [Movement ABC-2]. London, UK: The Psychological Corporation.
- Hirsch, C., John, M. T., Lautenschläger, C., & List, T. (2006). Mandibular jaw movement capacity in 10–17‐yr‐old children and adolescents: normative values and the influence of gender, age, and temporomandibular disorders. European journal of oral sciences, 114(6), 465-470.
- Hurley-Wallace, A., Wood, C., Franck, L. S., Howard, R. F., & Liossi, C. (2019). Paediatric pain education for health care professionals. Pain reports, 4(1).
- Jones, M. A. (1992). Clinical reasoning in manual therapy. Physical therapy, 72(12), 875-884.
- Jones, M. A., & Rivett, D. A. (2018). Clinical Reasoning in Musculoskeletal Practice-E-Book. Elsevier Health Sciences.
- Kröner-Herwig, B., Heinrich, M., & Morris, L. (2007). Headache in German children and adolescents: a population-based epidemiological study. Cephalalgia, 27(6), 519-527.
- Lambourne, C., Lampasso, J., Buchanan Jr, W. C., Dunford, R., & McCall, W. (2007). Malocclusion as a risk factor in the etiology of headaches in children and adolescents. American Journal of Orthodontics and Dentofacial Orthopedics, 132(6), 754-761.
- Langhagen, T., Schroeder, A. S., Rettinger, N., Borggraefe, I., & Jahn, K. (2013). Migraine-related vertigo and somatoform vertigo frequently occur in children and are often associated. Neuropediatrics, 44(01), 055-058.
- Lewis, D. W. (2007). Headaches in children and adolescents. Current problems in pediatric and adolescent health care, 37(6), 207-246.
- Li, B. U., & Balint, J. P. (2000). Cyclic vomiting syndrome: evolution in our understanding of a brain-gut disorder. Advances in pediatrics, 47, 117-160.
- Lindskog, U., Ödkvist, L., Noaksson, L., & Wallquist, J. (1999). Benign paroxysmal vertigo in childhood: a long‐term follow‐up. Headache: The Journal of Head and Face Pain, 39(1), 33-37.
- Locher, C., Kossowsky, J., Koechlin, H., Lam, T. L., Barthel, J., Berde, C. B., ... & Meissner, K. (2020). Efficacy, safety, and acceptability of pharmacologic treatments for pediatric migraine prophylaxis: a systematic review and network meta-analysis. JAMA pediatrics, 174(4), 341-349.
- Minen, M. T., De Dhaem, O. B., Van Diest, A. K., Powers, S., Schwedt, T. J., Lipton, R., & Silbersweig, D. (2016). Migraine and its psychiatric comorbidities. Journal of Neurology, Neurosurgery & Psychiatry, 87(7), 741-749.
- Mönch-Tegeter, I., von Piekartz, H. (2013). Haben Kinder mit Migräne veränderte kraniozervikale-vestibuläre Qualitäten im Vergleich zu Kindern ohne Kopfschmerzen?. manuelletherapie, 17(05), 223-232.
- Noseda, R., Kainz, V., Borsook, D., & Burstein, R. (2014). Neurochemical pathways that converge on thalamic trigeminovascular neurons: potential substrate for modulation of migraine by sleep, food intake, stress and anxiety. PLoS One, 9(8), e103929.
- Pereira, L. J., Costa, R. C., França, J. P., Pereira, S. M., & Castelo, P. M. (2009). Risk indicators for signs and symptoms of temporomandibular dysfunction in children. Journal of clinical pediatric dentistry, 34(1), 81-86.
- Pincus, T., Holt, N., Vogel, S., Underwood, M., Savage, R., Walsh, D. A., & Taylor, S. J. C. (2013). Cognitive and affective reassurance and patient outcomes in primary care: a systematic review. Pain®, 154(11), 2407-2416.
- Prakash, C., Staiano, A., Rothbaum, R. J., & Clouse, R. E. (2001). Similarities in cyclic vomiting syndrome across age groups. The American journal of gastroenterology, 96(3), 684-688.
- Rajapakse, D., Liossi, C., & Howard, R. F. (2014). Presentation and management of chronic pain. Archives of disease in childhood, 99(5), 474-480.
- Rosman, N. P., Douglass, L. M., Sharif, U. M., & Paolini, J. (2009). The neurology of benign paroxysmal torticollis of infancy: report of 10 new cases and review of the literature. Journal of child neurology, 24(2), 155-160.
- Rossi, L. N., Vajani, S., Cortinovis, I., Spreafico, F., & Menegazzo, L. (2008). Analysis of the International Classification of Headache Disorders for diagnosis of migraine and tension‐type headache in children. Developmental Medicine & Child Neurology, 50(4), 305-310.
- Shiri, S., Feintuch, U., Weiss, N., Pustilnik, A., Geffen, T., Kay, B., ... & Berger, I. (2013). A virtual reality system combined with biofeedback for treating pediatric chronic headache—a pilot study. Pain Medicine, 14(5), 621-627.
- Shulman, J., Conroy, C., Cybulski, A., Smith, K. R., Jervis, K., Johnson, H., ... & Sethna, N. F. (2020). Does intensive interdisciplinary pain treatment improve pediatric headache-related disability?. Disability and rehabilitation, 1-8.
- Singhi, S., Jacobs, H., & Gladstein, J. (2014). Pediatric headache: where have we been and where do we need to be. Headache: the Journal of Head and Face Pain, 54(5), 817-829.
- Slover, R., & Kent, S. (2015). Pediatric headaches. Advances in pediatrics, 62(1), 283-293.
- Spiri, D., Rinaldi, V. E., & Titomanlio, L. (2014). Pediatric migraine and episodic syndromes that may be associated with migraine. Italian journal of pediatrics, 40(1), 1-11.
- Trottier, E. D., Bailey, B., Lucas, N., & Lortie, A. (2013). Diagnosis of migraine in the pediatric emergency department. Pediatric Neurology, 49(1), 40-45.
- Lewis, D. W. (2007). Headaches in children and adolescents. Current problems in pediatric and adolescent health care, 37(6), 207-246.
- van der Meer, H. A., Visscher, C. M., Engelbert, R. H., Mulleners, W. M., Nijhuis–van der Sanden, M. W., & Speksnijder, C. M. (2018). Nederlandse versie. Headache Screening Questionnaire (HSQ). FysioPraxis; 9: 28-29.
- von Piekartz, H. J., Schouten, S., & Aufdemkampe, G. (2007). Neurodynamic responses in children with migraine or cervicogenic headache versus a control group. A comparative study. Manual therapy, 12(2), 153-160.
- Von Piekartz, H. V., & Mohr, G. (2014). Reduction of head and face pain by challenging lateralization and basic emotions: a proposal for future assessment and rehabilitation strategies. Journal of Manual & Manipulative Therapy, 22(1), 24-35.
- von Piekartz, H. J. (Ed.). (2015). Kiefer, Gesichts-und Zervikalregion: Neuromuskuloskeletals Assessment und Behandlungsstrategien. Thieme.
- Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasifard, M., ... & Abdollahi, M. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204-1222.
- WHO. World Health Organization. (2007). WHO child growth standards: head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age: methods and development. World Health Organization.

Manual Cranial Therapy
Cranial manual therapy means: assessment and treatment of the cranium..
Read more..

Pain Education
“pain neuroscience education (PNE)” or “Explain Pain” is a therapeutic tool...
Read more..

Headache (HA) in children
What can the (specialized) physical therapist mean for this pain suffering group..
Read more..

Assessment Bruxism
Assessment and Management of Bruxism by certificated CRAFTA® Physical Therapists
Read more..

Clinical classification of cranial neuropathies
Assessment and Treatment of cranial neuropathies driven by clinical classification..
Read more..

Functional Dysphonia
Functional Dysphonia (FD) is a condition characterized by voice problems in the absence of a physical laryngeal pathology.
Read more..

Body Image and Distorted Perception
Body Image and Distorted Perception of One's Own Body – What Does This Mean?
Read more..

TMD in Children
TMD affects not only adults, but it also occurs frequently in children and adolescents..
Read more..


