Understanding and Overcoming Vocal Impairments
Christian Voith, PT, MT (OMPT)
Harry von Piekartz, PhD, MSc, PT, MT (OMPT)

In the advanced courses of the CRAFTA education program, course members will encounter speech issues, with a particular emphasis on functional dysphonia (FD). FD is an often-underappreciated condition affecting individuals who intensely use their voice, whether professionally or otherwise. This brief outlines FD and provides a summary of what a certified CRAFTA Therapist can offer to patients dealing with this condition.
What is Functional Dysphonia?
Functional Dysphonia (FD) is a condition characterized by voice problems in the absence of a physical laryngeal pathology. It often manifests due to aberrant muscle contractions resulting in changes in voice quality (Roy and Bless 2000).
Clinically, it is expressed in a voice disorder characterized by abnormal vocal pitch, quality or volume and is often presented with ventral neck pain, hoarseness, and general vocal issues. Despite the absence of organic or pathological findings, it is suspected that laryngeal structures, musculature, and neural controls play a crucial role in the development of FD (Sama et al. 2001).
The primary feature of dysphonia is hoarseness and ventral neck and jaw pain. Patients may also experience sensations in the throat (such as pressure, scratching, burning, or a lump feeling) and pain in the larynx or pharyngeal area. Swallowing difficulties and other functional disorders, such as those occurring during speech, are also common. It's believed that functional voice disorders are often associated with muscular imbalances, especially in the shoulder, neck, jaw, and facial areas. A frequently affected muscle is the sternocleidomastoid (Friedrich et al. 2008; Mathieson et al. 2009).

Neuromusculoskeletal diagnosis in patients with FD includes a thorough examination of the larynx, head-neck-jaw region, posture, and abdominal muscle function, which falls under the purview of musculoskeletal therapists. For singers with FD, a systematic musculoskeletal assessment is recommended to establish a suitable treatment foundation and effective management of the disorder (Terney et al. 2021).
Functional dysphonia’s often occur in professions requiring high vocal performance, such as teachers, singers, lifeguards, actors or call center workers. Stress and psychological strain can also play a role, making people in high-stress jobs or life situations more susceptible to functional dysphonia’s (Bridger 1983; Chavan et al 2022).

A summary of the assessment content is provided.
Subjective Assessment
Questionnaires
Two specific questionnaires help assess contributing factors in voice dysfunctions and support further assessment and management:
- The Roughness, Breathiness, and Hoarseness (RBH) Index is a clinically established evaluation method in German-speaking countries, assessing roughness, breathability, and hoarseness of the voice (Moers et al. 2012).
- The Singing Voice Handicap Index (SVHI) developed by Cohen et al. (2007) consists of 36 statements focusing on self-assessment of the physical, emotional, social, and economic impacts of voice disorders in singing.
These questions may be employed to gain insights into the patient's impairment and participation, as well as to identify contributing and risk factors specific to the individual patient or client.
Additionally, special questions will be asked regarding voice usage, posture, and movement-related influences to gain an understanding of the extent to which the neuromusculoskeletal system plays a role in the client/patient's problem. Subjective questions will also be posed to identify potential "red flag" signals.
Physical Examination

Inspection
- Posture and movement control of the orofacial-cervical region: Posture, especially upright posture, and head position, are crucial for good voice quality and can contribute to discomfort if not optimal.
- Head position is assessed for anteroposition or posterior rotation of the cranium and influence on voice function.
- Changes in position in the craniocervical area influence voice production through anatomical/functional changes between the larynx, hyoid, epiglottis, soft palate, skull base, craniofacial skeleton, and cervical spine. Altering head position also changes the pharyngeal space, affecting resonance development.
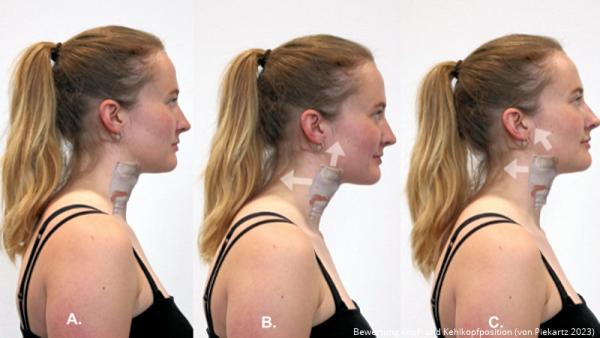
- Larynx position is specifically observed from ventral and lateral viewpoints and has a passive correction influence on the voice quality and pain.
- Shoulder elevation/protraction is evaluated bilaterally using the Clavicle Horizontal Angle (CHA). Normally, the clavicle's angle with the horizontal line is about 15 degrees. Asymmetry of the shoulders and too much elevation of shoulder can influence the pharynx function.
- Thorax position: Is breathing predominantly occurring in the costosternal area, or is abdominal breathing also present?
- Abdominal muscle activities and assessment: Evaluated to see if waist narrowing occurs gradually during expiration without pelvic movement, followed by ribcage movement. How is the activity of the transversus abdominus muscle during pitch? The abdominal muscles, along with the diaphragm, regulate exhalation flow and hence play a contributing role in dysphonia’s.
- Breathing patterns and compensatory movements: Vocal tests (e.g., glissando, crescendo) in different positions are used to observe breathing localization and compensatory movements.
- Tongue function screening tests: Assessing strength, coordination and endurance, and sensory response of the tongue to determine if it is a contributing factor.
- Active Tests of Pharynx/Hyoid Function: During swallowing, the larynx's capacity for elevation and depression is examined, and the patient's behavior is monitored during speaking and singing. Observations focus on any compensatory movements. Similar assessments are conducted for the hyoid bone, particularly examining its movement during vocal activities, especially when the tongue is engaged.
- Passive tests: Additional movements of the hyoid, thyroid, and cricoid are tested for abnormal resistance, protective spasm, and patients' subjective sensory sensations like pain or discomfort.
- Cranial nervous system: Due to the innervation of the larynx and the topography of nerves in the ventral neck area, particularly the Vagus nerve and the Glossopharyngeal nerve are tested for their conduction, palpation, and neurodynamic.
- Palpation of the ventral neck region: Typically, the hyoid, thyroid, and cricoid are palpated for sensitivity and position, as well as the supra- and infrahyoid muscles and the extrinsic laryngeal musculature (see also YouTube https://www.youtube.com/watch?v=jjq1NueKF4w&t=2s).
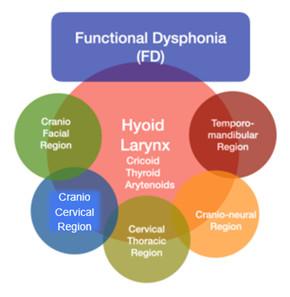
The source of symptoms that can be examined and treated by a specialized musculoskeletal therapist during FD, due to functional connections between the hyoid/larynx and surrounding regions (own resources Advanced courses CRAFTA).
Neuromusculoskeletal Treatment of Functional Dysphonia (FD)
Based on reflections from the subjective and physical assessments, a treatment/ management plan is formulated, comprising
- DIRECT voice therapy which means actively working on the voice itselfthrough
- Manual therapy of the larynx, orofacial and neck region (Hands on)
- Active (vocal) exercise improving the individual voice (Hands off)
- INDIRECT voice therapy like education of voice care, behavior, and life style factors.
a. Manual therapy (Hand on)
- Hyoid and larynx mobilizations: Especially larynx mobilization and relaxation of the suprahyoid muscles, combined with posture adjustments, seem to significantly improve the function of the vocal tract in occupational dysphonia.
- Trigger point treatment: Increased muscle tension in the larynx can inhibit normal speech production. Muscle stretching and light transverse movements on the trigger points of the Cricothyroid or Thyrohyoid muscles can result in significant improvement.
- Neurodynamic mobilization: Local methods for the hyoid and cricoid in neurodynamic positions can have rapid positive effects on neuralgia of the Superior Laryngeal Nerve.
- Secondary dysfunctions (primarily myofascial) in the neck and masticatory system.

b. Hands off
- Posture Correction: Since posture significantly impacts voice production, therapists can work on correcting and improving the patient's posture, particularly focusing on the neck, shoulders, and spinal alignment.
- Vocal Function Exercises: These are specific exercises aimed at strengthening the vocal cords, improving their flexibility, and enhancing voice quality.
- Breathing Exercises: Techniques for controlled breathing may be introduced to enhance voice control and alleviate stress on the vocal cords, particularly focusing on abdominal respiration.
- Active therapy focused on strengthen and coordination: Targeted exercises to strengthen and coordinate the muscles involved in voice production, including those in the face, neck, retraction muscles of the shoulder and respiratory system.
- Acoustic Biofeedback: Using technology to provide real-time feedback on voice pitch, volume, and quality, helping the patient to adjust and improve their vocal function.
- Orofacial Motor Control Exercises: To improve the coordination of muscles and movements involved in speech production.

- Education and Counseling: Educating patients about FD, including voice care techniques, lifestyle changes, and stress management strategies to reduce the impact of environmental and emotional factors on their condition.
By utilizing a combination of these approaches, physical therapists can help patients with functional dysphonia to improve their voice function and quality of life.
Evidence of neuromusculoskeletal treatment of functional dysphonia
The literature on the treatment of functional dysphonia, which refers to musculoskeletal approaches, indicates a multi-faceted approach.
A Cochrane systematic review evaluating treatments for functional dysphonia in adults found that a combination of direct and indirect voice therapy improved vocal functioning more effectively than no intervention. However, the effectiveness of direct voice therapy (actively working on the voice itself through vocal exercises and techniques) alone or indirect voice therapy (like education of voice care, behavior and life style factors) alone was not established. The review also assessed other treatments like pharmacological interventions and vocal hygiene instructions, but these did not show significant additional benefits. It highlights the importance of early and accurate diagnosis for effective treatment and suggests a need for further research on the specific effectiveness of musculoskeletal treatments within this context (Ruotsalainen et al 2007).
In another systematic review and meta-analysis for treating functional dysphonia and preventing voice disorders was found that a combination of direct and indirect voice therapy significantly improves vocal functioning in adults with functional dysphonia, with effects lasting at least 14 weeks. However, the review also found no evidence supporting the effectiveness of voice training in preventing voice disorders (Jani et al 2008).
Based on literature research and the knowledge of the authors of this statement, no recent literature review has been conducted regarding neuromusculoskeletal treatment of functional dysphonia (FD).
In this external evidence in mind, multidisciplinary collaboration is crucial. Therefore, it should be strongly promoted in consensus with ENT doctors, speech therapists, and voice teachers due to the growing prevalence of this patient group. A CRAFTA® therapist treats dysfunction and pain in this area based on the best current clinical and scientific knowledge. Patient complaints and dysfunctions are individually examined and treated, considering the medical diagnosis.

References
Here are the references sorted alphabetically in APA style:
- Behlau, M., Madazio, G. and Oliveira, G., 2015. Functional dysphonia: strategies to improve patient outcomes. Patient related outcome measures, pp.243-253.
- Bridger MWM, Epstein R. Functional voice disorders. A review of 109 patients. J Laryngol Otol. 1983, 97:1145–1148.
- Chavan, A., Maran, R. and Chavan, G., 2022. Dysphonia: Epidemiology, Diagnosis and Risk Factors at Tertiary Health Care Center. Indian Journal of Otolaryngology and Head & Neck Surgery, 74(Suppl 3), pp.5611-5615.
- Cohen, S.M., Jacobson, B.H., Garrett, C.G., Noordzij, J.P., Stewart, M.G., Attia, A., Ossoff, R.H. and Cleveland, T.F., 2007. Creation and validation of the singing voice handicap index. Annals of Otology, Rhinology & Laryngology, 116(6), pp.402-406.
- Friedrich G, Bigenzahn W, Zorowka P. Phoniatrie und Pädaudiologie: Einführung in die medizinischen, psychologischen und linguistischen Grundlagen von Stimme, Sprache und Gehör, 4.Auflage, Bern: Huber Verlag, 2008.
- Jani, R., Jaana, S., Laura, L. and Jos, V., 2008. Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngology—head and Neck Surgery, 138(5), pp.557-565.
- Mathieson L, Hirani SP, Epstein R, Baken RJ, Wood G, Rubin JS. Laryngeal manual therapy: a preliminary study to examine its treatment effects in the management of muscle tension dysphonia, Journal of voice 2009, 23 (3): 353-366.
- Moers, C., Möbius, B., Rosanowski, F., Nöth, E., Eysholdt, U. and Haderlein, T.,Vowel-and text-based cepstral analysis of chronic hoarseness. Journal of Voice, 26(4), pp.416-424.
- Roy, N. and Bless, D.M., 2000. Personality traits and psychological factors in voice pathology: A foundation for future research. Journal of Speech, Language, and Hearing Research, 43(3), pp.737-748.
- Ruotsalainen, J. H., Sellman, J., Lehto, L., Jauhiainen, M., & Verbeek, J. H. (2007). Interventions for treating functional dysphonia in adults. Cochrane Database of Systematic Reviews, (3).
- Sama, A., Carding, P.N., Price, S., Kelly, P. and Wilson, J.A., 2001. The clinical features of functional dysphonia. The Laryngoscope, 111(3), pp.458-463.
- Terney, W.S., Xiao, R. and Milstein, C.F., 2021. Characterization of functional dysphonia: pre-and post-treatment findings. The Laryngoscope, 131(6), pp.E1957- E1964.
- von Piekartz, H.J., 2023. Spezialisierte muskuloskelettale Therapie bei Sängerinnen und Sängern mit Dysphonie. MSK–Muskuloskelettale Physiotherapie, 27(01), pp.17- 26.
- Voith C, von Piekartz, H., 2017. Neuromuskuloskeletale Untersuchung und Behandlung bei funktioneller Dysphonie. Manuelle Therapie, 21(05), pp.214-220.

Manual Cranial Therapy
Cranial manual therapy means: assessment and treatment of the cranium..
Read more..

Pain Education
“pain neuroscience education (PNE)” or “Explain Pain” is a therapeutic tool...
Read more..

Headache (HA) in children
What can the (specialized) physical therapist mean for this pain suffering group..
Read more..

Assessment Bruxism
Assessment and Management of Bruxism by certificated CRAFTA® Physical Therapists
Read more..

Clinical classification of cranial neuropathies
Assessment and Treatment of cranial neuropathies driven by clinical classification..
Read more..

Functional Dysphonia
Functional Dysphonia (FD) is a condition characterized by voice problems in the absence of a physical laryngeal pathology.
Read more..

Body Image and Distorted Perception
Body Image and Distorted Perception of One's Own Body – What Does This Mean?
Read more..

TMD in Children
TMD affects not only adults, but it also occurs frequently in children and adolescents..
Read more..


