Willkommen bei CRAFTA®
Es ist unmöglich, sich die Diagnose und Behandlung von Kopf- und Gesichtsschmerzen mit ihren interaktiven Charakteristika ohne einen interdisziplinären Ansatz vorzustellen.Trotz aller Bemühungen sind die Behandler bei der Behandlung der Beschwerden der Patienten immer noch allein gelassen.
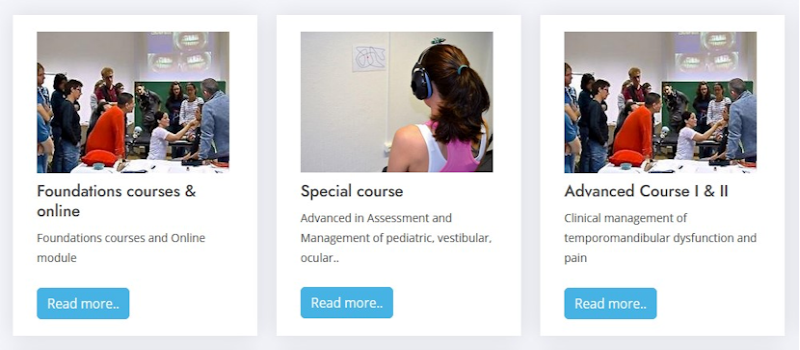
Das CRAFTA®-Ausbildungsprogramm ist patientenzentriert und wird den Anforderungen kritisch hinterfragender Ärzte und Therapeuten sowie der eher praktisch denkenden Kollegen gerecht.
Neuesten Nachrichten

Helping or Harming? CRAFTA® Response to the Pediatric Manual Therapy Debate
CRAFTA® BlogCRAFTA® curriculum
Mehr lesen..
CRAFTA-Webinare
CRAFTA® newsWir freuen uns, Sie ab dem Jahr 2025 zu einer Reihe dynamischer, interaktiver und kostenloser Webinare einzuladen!
Mehr lesen..
Hat die IFOMPT den Kopf verloren?
CRAFTA® BlogIn diesem Fall für Orofaciale (muskuloskelettale) Therapie
Mehr lesen..
Online Course for Temporomandibular Disorders
CRAFTA® BlogMr. Kraus is pleased to offer his course online: “Evaluation and Management of TMD with Cervical Spine Considerations”.
Mehr lesen..
An introduction into the Orofacial-Cervical Complex
CRAFTA® newsFREE - Warming up for the 5th CRAFTA CONGRESS
Mehr lesen..
5th Internat. CRAFTA® Congress ́24 SCHEDULE
CRAFTA® newsSCHEDULE - Update October 5th 2023
Mehr lesen..Unser Team

Pr. Dr. Harry von Piekartz
TEACHER - Harry J.M. von Piekartz hat 1985 die Ausbildung zum Physiotherapeuten an der Niederländischen Hochschule Enschede abgeschlossen.1988 hat er seine Ausbildung..
Mehr lesen..

Marisa Hoffmann
TEACHER - Marisa Hoffmann beendete Ihr Physiotherapie Studium im Jahr 2005 an der Europa Fachhochschule Fresenius, Idstein, in Kooperation mit der Hogeschool Utrecht. Im Anschluss..
Mehr lesen..

Michiel Trouw
TEACHER - Michiel Trouw (*1968) hat sein Studium der Physiotherapie an der Fachhochschule in Utrecht (Niederlande) im Jahre 1992 beendet. Er hat danach die MT-Ausbildung gemacht (OMT/ IFOMT)..
Mehr lesen..

Daniela von Piekartz
TEACHER - Daniela von Piekartz-Doppelhofer hat ihre Physiotherapie Ausbildung in 1996 an der Universitätsklinik in Graz (Österreich) abgeschlossen. Sie hat verschiedene Fortbildungen besucht..
Mehr lesen..